Chapter 13. Circulatory system
Higher category: 【Biology】 Biology Index
2. Blood Composition and Function
3. Circulatory System and Heart
1. Circulatory System
⑴ Types of Circulatory Systems
① Open Circulatory System
○ Organisms: Arthropods and mollusks
○ Simplicity: No capillaries; no clear distinction between hemolymph and interstitial fluid
○ Efficiency: Low hydraulic pressure saves energy; no need to form capillary networks, making it easier to build and maintain the circulatory system
② Closed Circulatory System
○ Organisms: Annelids, cephalopods, vertebrates, and other large or highly mobile organisms
○ Complexity: Presence of capillaries creates a distinction between blood and interstitial fluid
○ Efficiency: High hydraulic pressure allows efficient delivery of oxygen and nutrients; osmotic pressure is maintained by large molecules in the blood, helping to regulate blood pressure
⑵ Circulatory System in Vertebrates (Cardiovascular System) – Closed Circulatory System
① Animals with high metabolic rates possess more complex blood vessels and a more powerful heart compared to those with lower metabolic rates
② The complexity and distribution of blood vessels in an organism are proportional to the metabolic activity of each organ
③ Fish (1 atrium, 1 ventricle) – Single Circulation
○ No separation between systemic and pulmonary circulation; blood must pass through two capillary beds before returning to the heart, limiting blood flow speed.
○ Maintains necessary blood flow via skeletal muscle activity.
○ Only deoxygenated blood flows through the heart.
④ Amphibians (2 atria, 1 ventricle) – Double Circulation
○ Systemic and pulmonary circulations are separated, allowing more blood supply to the brain and muscles; however, mixing of oxygenated and deoxygenated blood reduces efficiency
○ To compensate for lower oxygen efficiency, a cutaneous circulation system is developed
⑤ Reptiles (2 atria, partially divided 2 ventricles) – Double Circulation
○ Less mixing of oxygenated and deoxygenated blood improves the efficiency of material exchange
⑥ Birds and Mammals (2 atria, fully divided 2 ventricles) – Double Circulation
○ Complete separation of oxygenated and deoxygenated blood enables efficient material exchange
○ This system supports endothermic animals, which consume approximately 10 times more energy than ectotherms of the same size
⑦ Human Circulatory System
○ Systemic circulation: Left ventricle → Aorta → Whole body (capillaries) → Vena cava → Right atrium
○ Pulmonary circulation: Right ventricle → Pulmonary artery → Lungs (capillaries) → Pulmonary vein → Left atrium
2. Blood composition and function
⑴ Blood centrifugation: Separate blood by component
① Centrifugation with Anticoagulant: Separated red blood cells, soft layers, and plasma from below to top
○ Soft layer (buffy coat): leucocytes + platelets
○ Plasma: Liquid composition of blood
② Centrifugation without anticoagulant: Separated into blood clots and serum from below to top
○ Blood clot: Ingredients of coagulated blood, red blood cells + leucocytes + platelets + blood coagulation factors
○ Serum: Liquid components remaining after blood clotting, removal of fibrinogen and other components from plasma
○ Cellular elements are entangled by fibrinogen in plasma
③ Erythrocyte volume fraction (hematocrit): Ratio of red blood cell volume to total blood volume
○ Normal adult man: 0.41 to 0.51
○ Normal adult woman: 0.36 to 0.45
○ Why men use power more than women
○ Anemic people have small hematocrit
○ Viscosity is proportional to erythrocyte volume fraction
⑵ Composition of blood
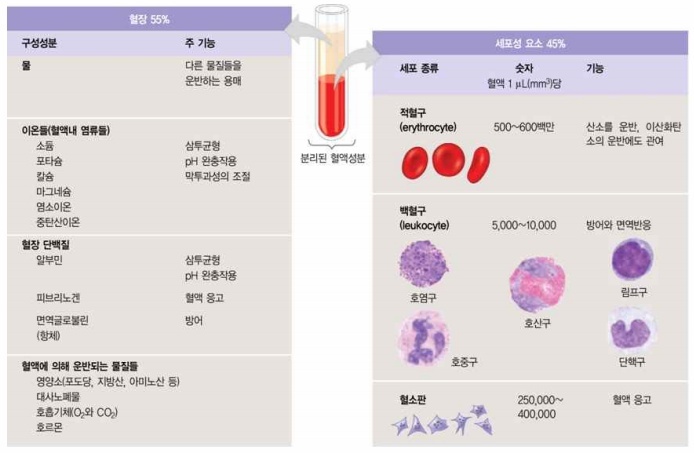
Figure 1. Composition of blood
① Blood: 7% of female weight, 8% of male weight
② Blood = plasma (55%) + cellular component (45%)
○ The amount of blood in a person with a body weight of 70 kg is about 5 L.
③ Plasma = Water (92%) + Protein (7%) + Other (1%)
○ Water: Solvents Carrying Other Materials
○ Na+, K+, Ca2+, Mg2+, Cl-, HCO3-: Osmotic balance, membrane permeability control
○ HCO3-, H2PO4-, Albumin, Hb (Bore effect): pH buffer
○ Fibrinogen: Blood clotting elements
○ Albumin: Osmotic balance. Involved in the transport of lipids. 60% of plasma proteins. Stored energy sources in plasma. 3.5 to 5 g / dl. Half-life of 20 days.
○ Globulin: It has a large molecular weight like albumin, so it can’t escape capillaries, increasing osmotic pressure in blood vessels
○ Immunoglobulins (antibodies), interferon: Defensive function, acting faster than NK cells
○ Lipoprotein: Carrying fat
○ Hormone binding protein: Especially carrying fat-soluble hormones
○ Transferrin: Iron-carrying protein
○ Nutrients, Metabolic Wastes, Respiratory Gases (O2, CO2), Hormones
④ Cellular elements
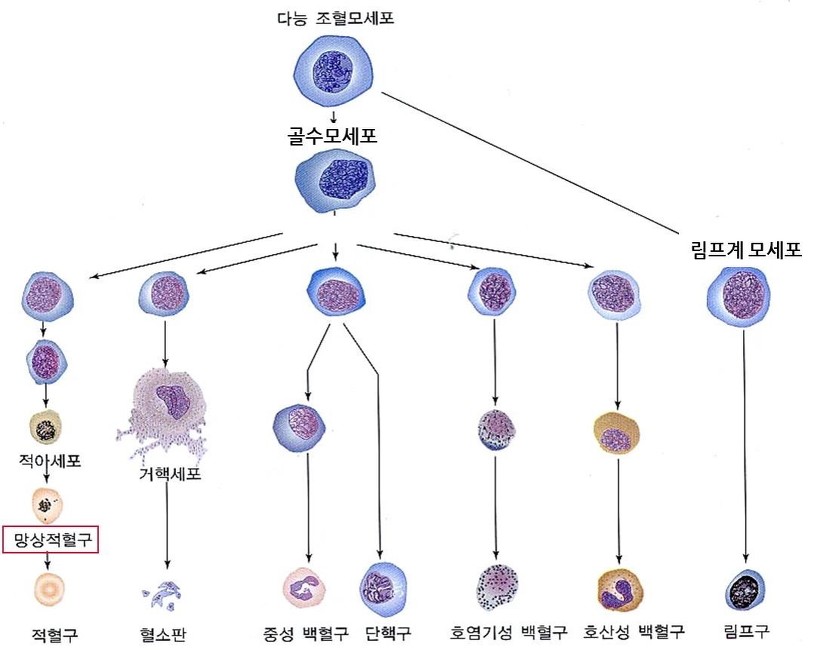
Figure 2. Types of Cellular Elements
⑶ Cellular elements: Red blood cells
① Structure: Concave, flexible disc-shaped cells on both sides filled with hemoglobin
○ A concave disc in the middle: Increased gas exchange efficiency by increasing the contact area between oxygen and red blood cells
○ Structure that can be folded and crumpled, making it easier to pass narrow capillaries
○ Hemoglobin is about 3 million per red blood cell
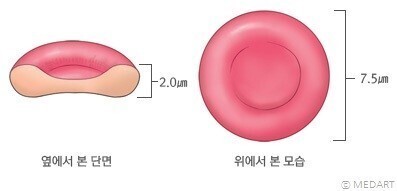
Figure 3. Type of red blood cells
○ Hemoglobin: The blood is red because it contains iron
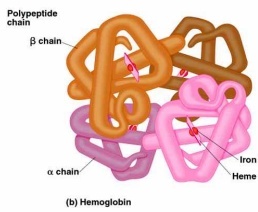
Figure 4. Structure of hemoglobin
② Function
○ Hemoglobin has the ability to bind to O2, which can carry oxygen
○ Erythrocytes are also involved in the transport of CO2
③ Production
○ Derived from bone marrow stem cells (or myeloid cells) in the ribs, thorax, pelvis, vertebrae, etc.
○ Erythroblast: A precursor cell of red blood cells.
○ During fetal period, red blood cells are produced from liver, spleen and bone marrow
○ 5 to 6 million pieces per mm3
○ 84% of human cells are red blood cells
○ Erythropoietin (EPO) produced by the kidney regulates red blood cell production
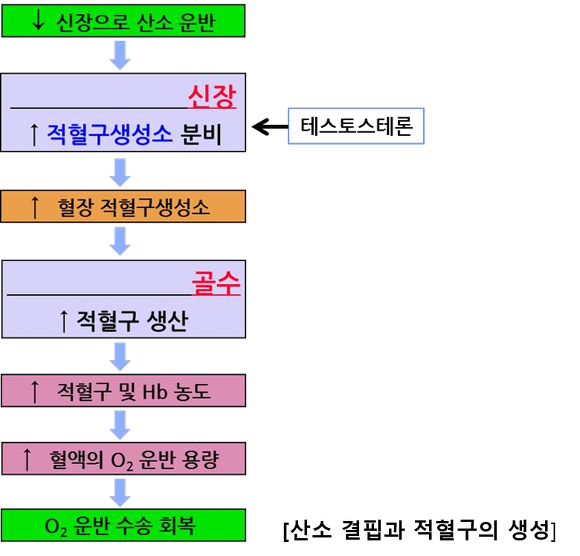
Figure 5. Oxygen deficiency and red blood cell production
④ Maturity: Other organelles are destroyed when the amount of hemoglobin in red blood cells reaches 30%
○ No oxygen consumption due to mitochondria removal during maturation and lactic acid fermentation to produce ATP
○ Only glucose is used as an energy source
○ Mammalia: Lack of nucleus, capable of containing large amounts of hemoglobin
○ Remainder: Nucleated cells
⑤ Place of destruction: Liver, Spleen
○ Erythrocyte lifespan: About 120 days
○ Spleen damage in sickle cell anemia
○ Spleen: Located in the back of the stomach, and it is able to produce leucocytes and destroy waste red blood cells.
○ Bile formation with bilirubin produced as a result of destroying red blood cells
⑥ Evolution Theory: Number of hemoglobin amino acids that differ from humans
○ Gorilla (1), Rhesus Macaque (8), Dog (15), Horse (25), Chicken (45), Frog (67), Hyperoartia (125)
⑷ Cellular elements: leucocytes (white blood cell)
① Originated from bone marrow stem cells, 5,000 to 10,000 per 1 mm3
② life span: 100 to 200 days
③ Characteristic
○ Unlike red blood cells, they also exist in intracellular and lymphatic fluids
○ Nucleus is present and used for karyotyping
○ The shape is not constant and amoeba movement
○ Swarming: Free movement within tissue
④ Production: Produced by colony stimulating factor (CSF) produced by endothelial cells, bone marrow fibroblasts and other leucocytes
⑤ Granulocyte: Phagocytosis, pus formation, allergic reactions, inflammatory reactions
○ Main feature: High density due to many polymorphonucleus and granules
○ Classified into neutrophils, eosinophils, basophils according to dyes for staining granulocytes
○ Neutrophils
○ Function: Antibody-Coated Pathogen Phagocytosis
○ Distribution: Account for 60-65% of total leucocytes. 12-14 μm
○ Granule form: Forming three lumps
○ Eosinophils
○ Function: Antibody-coated parasite death and allergic hypersensitivity involvement
○ Distribution: Account for 1% of total leucocytes
○ Shape: 2 lumps formed. Relatively large granules. 12 to 17 μm
○ Dyed red by Eosin.
○ Basophil neutrophils (basophils)
○ Function: Histamine and heparin release promotes T lymphocyte development
○ Distribution: Account for 0.2% of total leucocytes.
○ Shape: Dispersed granules, large granules, 14 ~ 16 ㎛
○ Dyed in dark purple by methylene blue
⑥ Mast cells: Release of histamine, leukotriene, etc., due to damage or antigen binding
○ Refers to basophilic leucocytes that act on tissue cells
⑦ Monocytes: Phagocytic cells. They make up about 4% of all white blood cells. Size: ~20 µm
○ Monocytes originate from hematopoietic stem cells located in the bone marrow.
○ Type 1: Macrophages
○ Type 2: Foreign body giant cells
○ Monocytes differentiate into macrophages and dendritic cells.
⑧ Macrophages
○ Engulf and digest microorganisms, present antigens, and activate T lymphocytes
○ Microglia in the brain are also a type of macrophage
○ Classification 1: Based on Function
○ 1-1. M1 Macrophages (Classically Activated or Inflammatory Macrophages)
○ Pro-inflammatory cells: Involved in cell death and anti-tumoral activity.
○ Elongation factor: Ratio of long axis to short axis is close to 1.
○ Cytokines that induce M1 type: TLR, TNF-α, IFN-γ, CSF2, LPS, STAT1, IRF5, IL-17A
○ Cytokines secreted by M1 type: IL-6, IL-8, IL-23p40, TNF-α, IL-1β, IL-12p70, IL-12p40, IFN-γ
○ Gene markers of M1 type: HLA-DR, CD11c, CD86, iNOS, pSTAT1, IL-12, MHC-II, CD80, 27E10, CCL2, S100A8, S100A9
○ 1-2. M2 Macrophages (Alternatively Activated or Anti-inflammatory Macrophages)
○ Anti-inflammatory cells: Involved in tissue repair and pro-tumoral activity.
○ Elongation factor: High ratio of long axis to short axis.
○ Cytokines that induce M2 type: IL-4, IL-10, IL-13, TGF-β, PGE2, STAT3, STAT6, IRF4
○ Cytokines secreted by M2 type: IL-10
○ Gene markers of M2 type: CD68, CD163, CD204, CD206, VEGF, cMAF, ARG1, YM1, CCL20, CCL22, IDO1
○ Most tumor-associated macrophages (TAMs) are of the M2 type.
○ Classification 2: Based on Tissue Location
○ Kupffer cells: Macrophages located in liver capillaries.
○ Part of the innate immune system known as the reticuloendothelial system (RES).
○ The only macrophages located within blood vessels.
○ Splenocytes: Located in the spleen.
○ BMDM (Bone-Marrow-Derived Macrophage): Located in bone.
○ Dust cells: Located in the lungs.
○ Microglial cells: Located in the brain.
○ TAM (Tumor-Associated Macrophages): Found within tumor microenvironments.
| Function (M1-like TAM) | M1-like TAM | Function (M2-like TAM) | M2-like TAM |
|---|---|---|---|
| Immune activation (Th1 and NK) | TNF-α, NO, IL-23, IFN-γ, MHC class II, IL-1β, CXCL10 | Angiogenesis | VEGF, FGF, CXCL8, Tie2, hypoxia |
| Phagocytosis of tumor cells | — | EMT (epithelial mesenchymal transition) | TGF-β |
| Apoptosis of tumor cells | TNF-α, FasL | Immune Suppression (Treg or Th2) | PD-1, PD-L1, IL-10, TGF-β, IDO 1/2, arginase |
| Tissue damage | ROS, iNOS | Tissue remodeling metastasis | MMPs, uPAR, cathepsins |
| Maturation of APC | IL-12 | Tumoral growth factors | EGF, FGF, TGF-β, PDGF |
Table 1. M1-like TAM과 M2-like TAM
⑨ Dendritic cells: Antigen Expression in T Lymphocytes
⑩ Lymphocytes: B lymphocytes, T lymphocytes, natural killer cells, accounting for 20-35% of all leucocytes, 6-9 μm
○ Lymphocytes do not move into the blood vessels and only work within the lymph vessels
○ High percentage of nuclei compared to other leucocytes
⑷ Cellular elements: Platelets
① A fragment of the cytoplasm of bone marrow special cells (bone marrow megakaryocytes)
○ Characteristic: No nucleus, and involved in blood coagulation
○ Uneven in shape and very small compared to erythrocytes and leucocytes
② Produce
○ 250,000 to 400,000 cells per mm3
○ Produced by TPO (thrombopoietin) produced by the liver
③ Life span: 9-12 days
④ Function: Blood Coagulation
⑤ Anti-platelet agent
○ Aspirin
○ P2Y12 inhibitor: clopidogrel, prasugrel, ticagrelor, etc.
○ Tirofiban: glycoprotein Ⅱb / Ⅲa receptor inhibitor
○ HBA(hydroxybenzy alcohol): anti-inflammatory and anti-platelet activity
3. Circulatory system and heart
⑴ Structure of the heart
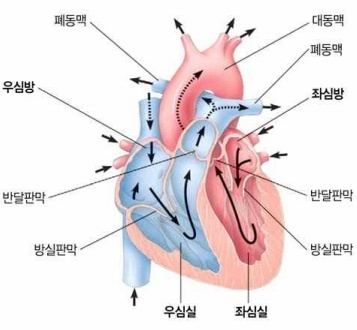
Figure 6. Structure of the heart
① The heart is located beneath the sternum and is about the size of a fist, mostly composed of cardiac muscle.
② It consists of the atrium, which receives blood, and the ventricle, which delivers blood: two atria and two ventricles for human.
③ The ventricles have a thicker muscle layer than the atria and have a stronger contractile force.
○ In particular, the left ventricle contracts with much stronger force, sending blood to each organ in the body
○ The left ventricle contracts more powerfully than the right ventricle, but the same amount of blood is released in one contraction
④ Valve: Four valves in the heart prevent blood from flowing back
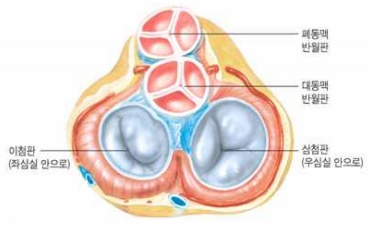
Figure 7. Valve structure
○ Atrioventricular valve: Between the atria and the ventricles, tricuspid and bicuspid
○ Meniscus valve: Between the ventricle and the artery
○ Abnormal sound (heart noise) occurs when blood is ejected through an incomplete valve when the valve is abnormal
⑵ Heart muscle
① Characteristic
○ High density of capillaries and mitochondria: Aerobic respiration
○ Red due to high myoglobin content
○ Nutrition: Fatty acids ≫ Glucose, lactic acid (∴ aerobic respiration only)
○ Coronary artery: Blood supply to heart muscle, lack of blood supply to heart muscle causes cardiac arrest, heart attack, myocardial infarction
② Pacemaker Potential of Autorhythmic Cells
○ Autorhythmic cells: Sinoatrial (SA) node (located in the right atrium), Atrioventricular (AV) node (located in the right atrium), Purkinje fibers
○ SA node: Generates pacemaker potentials without external electrical signals
○ AV node and Purkinje fibers: Amplify potentials when they receive external electrical signals
○ The SA node shortens the diastolic period and increases heart rate under sympathetic stimulation
○ The SA node lengthens the diastolic period and decreases heart rate under parasympathetic stimulation
○ The autonomic nerve that acts on the SA node is a branch of the vagus nerve (vagus n.)
○ Ventricular myocardium is influenced only by the sympathetic nervous system, which regulates stroke volume
⑶ Cardiac cycle: How the heart pumps and receives blood
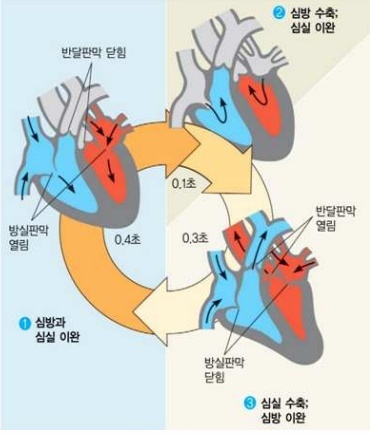
Figure 8. Cardiac cycle
① Pulse: Changes in blood vessels according to the cardiac cycle
② Systolic: Blood flow in the ventricles → arteries
③ Diastolic: Blood flow atrium → ventricles
④ Atrium, Ventricular Relaxation: Intravenous → Atrium → Ventricular. Bicuspids and tricuspids open. Meniscal valve closed (0.4 seconds)
⑤ Atrial contraction, ventricular relaxation: Atrial blood → ventricles, Bicuspids and tricuspids open, meniscus closed (0.1 second)
⑥ The delayed time (0.1 seconds) that prevents the atria and ventricles from contracting simultaneously originates from the atrioventricular (AV) delay.
⑦ Delayed time so that the atria and the ventricles do not contract at the same time (0.1 second) is due to the atrioventricular delay
⑧ Cardiac arrest
○ Cardiac arrest due to synchronization failure, fibrillation, arrhythmia
○ Synchronization by electric shock (re-defibrillation)
⑷ Electrocardiography (ECG)
① Summary
○ It represents the heartbeat as electrical signals and does not involve attaching electrodes directly to the heart; it is typically measured using 12 electrodes.
○ Divided into waves and segments
○ Wave: If it goes up above the baseline and then goes down
○ Segment: Baseline between two waves
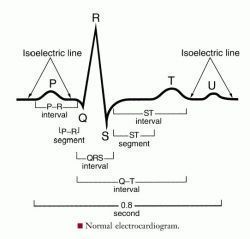
Figure 9. Electrocardiogram
○ Understanding ECG signals: Measures whether the electric field direction of the external electrodes aligns with the electric field direction within the heart.
② P wave: Depolarization of the SA node
○ Sinoatrial node (SA node): Tissue that voluntarily generates action potentials
○ A signal from the sinoatrial (SA) node causes atrial depolarization, leading to atrial contraction within 100 ms.
○ Initial state of valve: Atrioventricular valve open, meniscus valve closed
○ All cardiac muscle cells in the atria are connected by gap junctions, allowing the electrical signal from the sinoatrial (SA) node to rapidly spread throughout the entire atria.
③ P-Q interval: Atrioventricular (AV) Delay
○ AV delay: A delay of approximately 0.1 seconds in the action potential at the AV node, allowing time for blood to flow from the atria to the ventricles
○ Atrioventricular (AV) node
○ Gap junction pathway between the atria and ventricles
○ A pacemaker that receives signals from the SA node and generates fibrillation, synchronized with the SA node
④ Q point: The action potential reaches the bundle of His.
⑤ QRS Complex: Depolarization of the bundle of His and Purkinje fibers, i.e., ventricular depolarization
○ The bundle of His and Purkinje fibers are also considered pacemakers.
○ Depolarization of the Purkinje fibers → Ventricular depolarization → Triggers ventricular contraction.
○ As the ventricles contract, atrial repolarization occurs simultaneously → Leads to atrial relaxation.
○ Valve status: Atrioventricular (AV) valves are closed to prevent backflow from ventricles to atria; meniscus valves are also closed.
○ First heart sound (S1) occurs: The AV valves close, producing the “lub” sound
⑥ QRS-T Interval: The phase when the ventricles are actively contracting
○ Valve status: AV valves closed, meniscus valves open
○ After ventricular contraction, the meniscus valves open and blood is ejected into the arteries
○ Ventricular pressure rises and then begins to fall during this stage
⑦ T Wave: Ventricular repolarization, also includes a portion of the ST segment
○ Ventricular repolarization → Leads to ventricular relaxation
○ Valve status: To prevent blood from flowing back from arteries into ventricles, both AV and meniscus valves are closed
○ Second heart sound (S2) occurs: Meniscus valves close, producing the “dub” sound
⑧ U Wave
○ A small wave occurring after the T wave
○ It is presumed to be a relaxation signal caused by the vesicles following depolarization.
⑨ R-R Interval: Also referred to as the interval or heart rate
⑩ Summary of Valve Status
○ Lub Dub (≒ thump-thump): The sound of heart valves closing
○ Lub (at Q point): AV valves closing; meniscus valves closed
○ At S point: AV valves closed; meniscus valves opening
○ Dub (just before T wave): AV valves closed; meniscus valves closing
○ Just after T wave: AV valves opening; meniscus valves closed
⑸ Frank-Starling Curve: Ventricular Pressure-Volume Curve
① Isovolumetric Contraction
② Ventricular Ejection
③ Isovolumetric Relaxation
④ Ventricular Filling
⑤ Cardiac Cycle: Isovolumetric contraction → Ejection (0.3 s) → Isovolumetric relaxation → 0.4 s → 0.1 s
○ Reason for isovolumetric contraction: Due to the high pressure in the aorta
○ Reason for isovolumetric relaxation: To receive blood from the atria
⑹ Fetal heart
① Blood with gas and mass exchange in the placenta enters the right atrium through the inferior vena cava (93% circulatory circulation, 7% pulmonary circulation)
② Foramen ovale: An opening between the left and right atria that remains open during the fetal stage.
○ 60% of the blood going to the pulmonary artery goes to the aorta
○ At birth, the left atrium contractions are greater than the right atrium contractions, which push the lid of the foramen ovale and block it.
○ Incomplete closure of the foramen ovale (atrial septal defect): The foramen ovale fails to close properly, causing mixing of pulmonary and systemic circulation, leading to reduced exercise capacity (congenital).
③ Ductus arteriosus (Botallo’s duct): In the fetus, it allows blood from the pulmonary artery in fetus to flow into the aorta.
○ Incomplete closure of the ductus arteriosus (patent ductus arteriosus) (congenital)
4. Vascular system
⑴ blood vessel
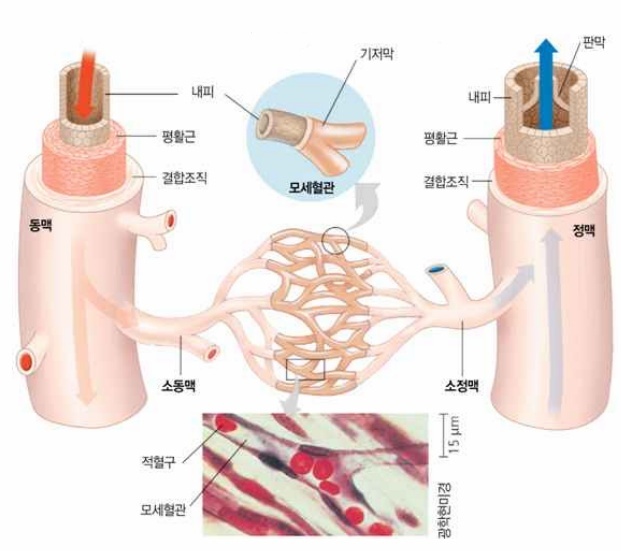
Figure 10. The structure of blood vessels
① Artery: Consists of three layers (intima, media, outer membrane), many elastic fibers and muscle fibers (smooth muscle), aorta (with 11% blood)
○ The proportion of elastic tissue is relatively higher than that of veins → elasticity ↑
○ With thick blood vessel walls, can withstand high blood pressure
○ The elasticity of the artery wall allows the artery to return to its original state and maintain high blood pressure when the heart relaxes
○ The aorta regulates its contraction and relaxation by itself
○ The arterioles are regulated in terms of constriction and dilation by the autonomic nervous system.
② Vein: Consists of three layers (intima, media, and outer membrane). Valves and muscle fibers (smooth muscle) are present. The vena cava and the venules (61% blood)
○ More than the artery and larger in diameter, holding more than half the blood in the circulatory system
○ The smallest blood flow resistance due to the largest radius among blood vessels
○ The walls are thinner and less elastic than those of arteries, and because the blood pressure is lower, valves are present to prevent backflow.
○ In addition to smooth muscle, there is a regulatory action of adjacent skeletal muscle
③ Capillaries
○ Capillary wall consists of a very thin layer of epithelial cells. No smooth muscle
○ Capillary pore (opening): Pores in a tube of endothelial cells. Not in the brain with strict control of BBB
○ Basal layer: Surrounded by endothelial cells, allowing for easy permeability, which facilitates the exchange of substances.
○ Hydrophobic substances and small hydrophilic substances: pass through the endothelial cell membrane by simple diffusion. Examples include carbon dioxide, water, glucose, and amino acids.
○ Large hydrophilic substances: Cross via transcytosis. In the liver and intestines, the gaps between endothelial cells are wide enough for proteins to pass through.
○ Cells located more than 100 μm away from capillaries will undergo cell death.
○ The diameter of alveolar capillaries is approximately 8 μm.
④ Blood pressure, total cross-sectional area, blood flow rate
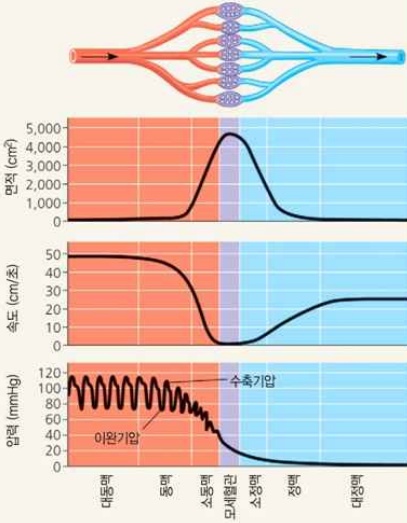 </center>
</center>
Figure 11. Blood pressure, total cross-sectional area, blood flow rate
○ Blood pressure: Arteries> Capillaries> Veins
○ Total cross-sectional area: Capillaries> Veins> Arteries
○ Blood flow rate: Arteries> Veins> Capillaries (∵ Continuous Equation)
○ Blood flow rate of arteries: 10 cm/s
○ Blood flow rate of veins: 0.05 cm/s
⑵ Blood pressure
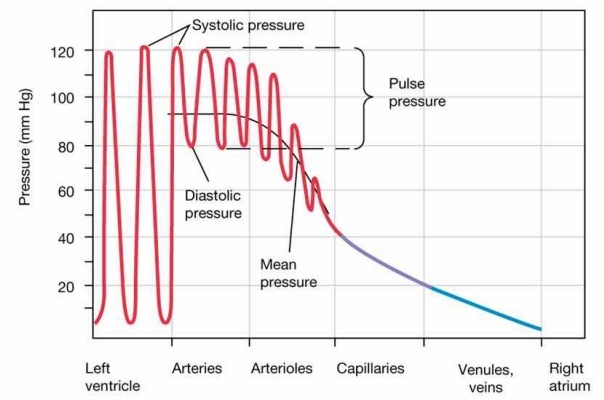
Figure 12. Blood pressure
① Ventricular Contraction Pressure (Max): One heart rate, release rate
○ Increased ventricular contraction pressure when the aorta decreases in distensibility
○ Increasing volume of single stroke increases ventricular contraction pressure
② Ventricular relaxation pressure (lowest): Peripheral circulation resistance, time to next systolic period
○ Decreased distensibility of the aorta reduces ventricular diastolic pressure
○ The volume of single stroke does not affect ventricular relaxation.
③ Pulse pressure (= systolic blood pressure-diastolic blood pressure) ← 1 stroke volume, elasticity of the aorta
④ Cardiac output = The volume of blood ejected from the ventricle for 1 minute = The volume change of the ventricles × heart rate for 1 minute
⑤ Blood pressure 120/80 (mmHg) is the pressure exerted in addition to the existing atmospheric pressure
⑥ Measurement of blood pressure
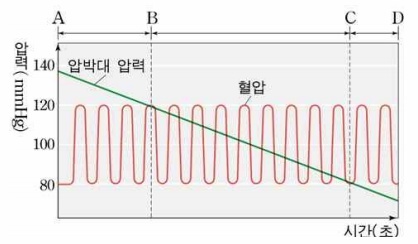
Figure 13. Measurement graph of blood pressure
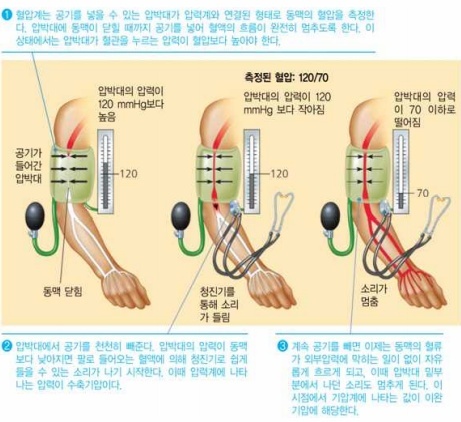
Figure 14. How to measure blood pressure
⑦ Blood pressure changes according to the cardiac cycle (CV physiology)
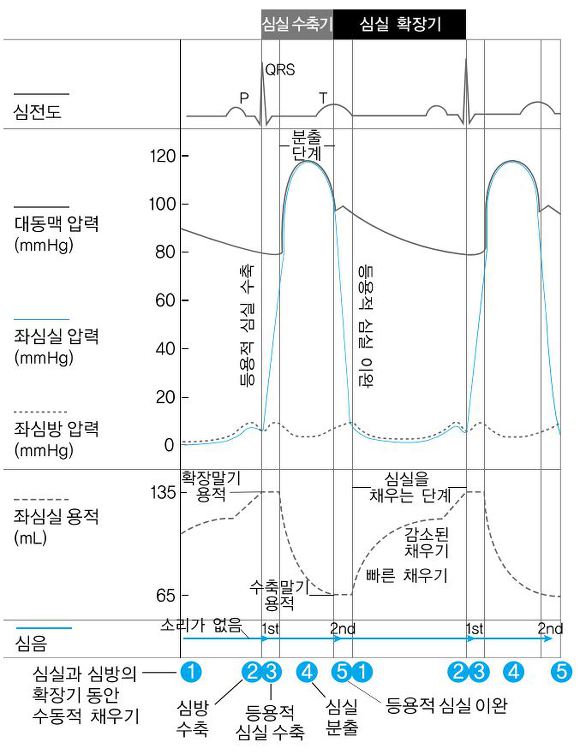
Figure 15. Blood pressure changes according to the cardiac cycle
○ The diastolic phase is approximately twice as long as the systolic phase.
○ The MAP (mean arterial pressure) is commonly calculated using the formula: MAP = (2 × diastolic + systolic) / 3
⑧ Blood pressure = Full load × Posterior load
○ Full load: Proportional to blood volume, long-term regulation, regulation in the kidneys
○ Posterior load: Proportional to capillary perfusion resistance, etc. Short-term regulation, controlled through contraction and relaxation of arterioles.
○ Vascular resistance

○ The body’s peripheral blood pressure is greater than the pressure of the heart because it has to go against gravity, and skeletal muscle is involved.
○ The typical blood pressure graph is for major blood vessels, and the above fact has not been confirmed.
⑶ Material transport through the walls of capillaries
① Capillaries have a single layer of cells and have the largest cross-sectional area, which is advantageous for mass exchange.
② Mass exchange method
○ Simple diffusion or facilitated diffusion: Oxygen, carbon dioxide, small molecules, some ionic material
○ Transcytosis: When moving large molecules (blood cells, proteins, etc.)
○ Movement through capillary pores
○ Active transport
○ Osmotic pressure
③ Driving force for mass exchange
○ Blood pressure
○ Blood osmotic pressure: Formed by large molecules remaining in the capillaries
⑷ Mechanism of blood flow to the heart through veins
① Disruptors of Vein Blood Flow
○ Veins have low blood pressure, which can reverse intravenous pressure depending on external conditions
○ Example. Gravity: Obstruct the flow of blood from bottom to top through an artery or vein
② Vein Blood Flow Mechanism: Helps blood flow to the heart
○ Valve: Prevent blood flow in the vein from reversed → Prevent blood flow reversed during muscle contraction and relaxation
○ Periodic contraction of smooth muscles surrounding the veins
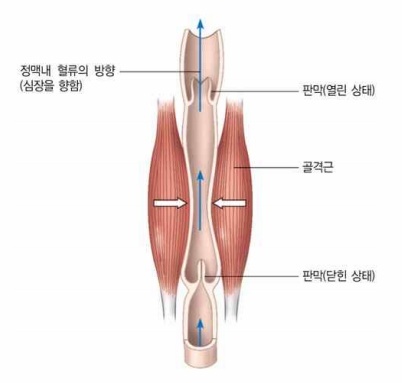
Figure 16. Vein Blood Flow Mechanism
○ When muscles contract, blood moves towards the heart
○ When the muscles relax, the valve closes to prevent blood backflow
○ Skeletal muscle contracting during exercise
○ Example. Efficacy in removing blood clots formed in veins when traveling long distances
○ Pressure changes in the chest cavity (negative pressure) dilate the vena cava around the heart
○ ↑ Venous pooling → ↑ Capillary pressure → ↑ Filtration → ↑ Interstitial fluid (tissue cells)
③ If an abnormality occurs in the valve of a vein, varicose veins develop: Blood stagnation, increased load, risk of pulmonary blood
⑸ Exchange of blood and tissue fluid
① Tissue fluid and lymphatic fluid
○ Tissue fluid
○ No plasma components, white blood cells, red blood cells and platelets from capillaries
○ Tissue fluid is secreted from the capillaries to supply the cells with the nutrients and materials they need
○ Function: Substance exchange with cells and immune function
○ Return of tissue: About 85% of tissue fluid goes to capillaries, and about 15% of tissue fluid goes to lymphatic vessels
○ Lymphatic fluid
○ Tissue fluid entering the lymphatic vessel
○ No blood cells, protein, etc.
② Exchange of blood and tissue fluid through capillaries
○ Hydrostatic pressure (capillary pressure) (Pc): Blood pressure acts as a force to push liquid
○ Plasma osmotic pressure (πp): High osmotic pressure acts as a force to draw water from tissue fluid
○ Tissue Fluid Hydrostatic Pressure (PIF)
○ Tissue Fluid Osmotic Pressure (πIF)
○ Frank-Starling law: Interstitial fluid (tissue exudate) = Kf(Pc - PIF) - σr(πp - πIF) ≒ (Pc - PIF) - (πp - πIF)
○ Net Filtration Pressure at End of Artery = (Pc-PIF)-(πp-πIF) = (35-0)-(28-3) = 10 mmHg
○ Net Filtration Pressure at End of Vein = (Pc-PIF)-(πp-πIF) = (15-0)-(28-3) = -10 mmHg
③ Return of liquid components through the lymphatic system: Lymph circulation is 1/3000 of cardiac output
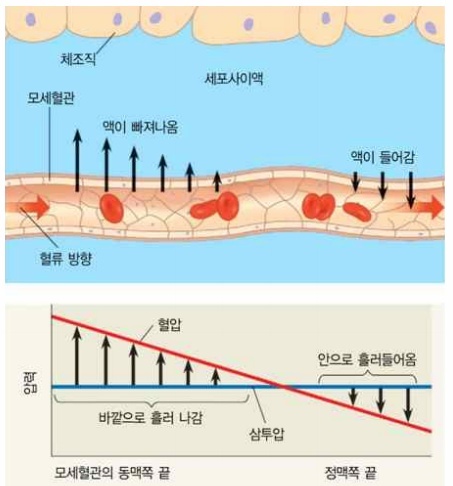
Figure 17. Blood and Lymphatic Exchange
○ Formation of the lymphatic system: The amount of water that has drained into the tissue fluid is greater than the amount of water that has entered the blood
○ Function
○ Lymph nodes: Exist along the main lymphatic vessels of birds and mammals. Various immune cells are located. Swelling upon infection.
○ Absorption of fat-soluble nutrients: Lymphatic system has thin walls and high permeability, allowing fat-soluble nutrients to move
○ Return to blood: Tissue fluid → blood
○ Lymph fluid recovery: Lymphatic capillaries → Thoracic duct → Superior vena cava → Subclavian vein → Heart
○ Backflow prevention mechanism
○ Lymphatic vessels have valves, like veins, that prevent backflow and ensure lymph flows into the thoracic duct.
○ Movement is driven by pressure from surrounding skeletal muscle contractions.
○ A phenomenon that occurs in the lymphatic system
○ Lymphocytes in lymph nodes enter the bloodstream through the thoracic duct.
○ Lymphocytes exit capillary walls, pass through interstitial spaces, and enter the lymphatic system.
○ Lymphatic vessels serve as pathways for nutrient transport from the small intestine to the bloodstream.
○ Blood cells cannot enter the lymphatic system.
④ Edema: An increase in interstitial fluid due to an imbalance in fluid recovery or abnormalities in the lymphatic system.
5. Blood flow control
⑴ Overview
① Neural signals, hormones, and chemicals serve as signals for blood flow regulation.
② The brain requires a constant and stable blood flow at all times.
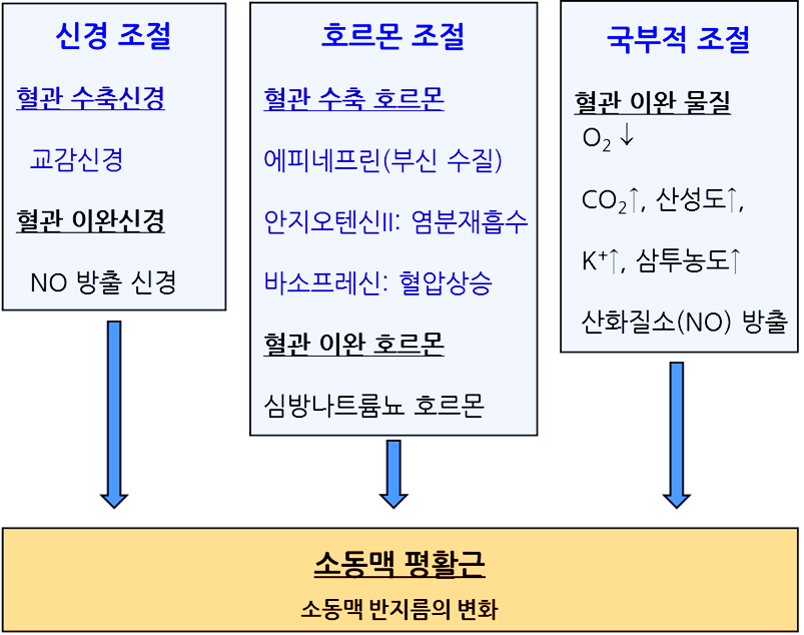
⑵ Overall control: Blood flow control
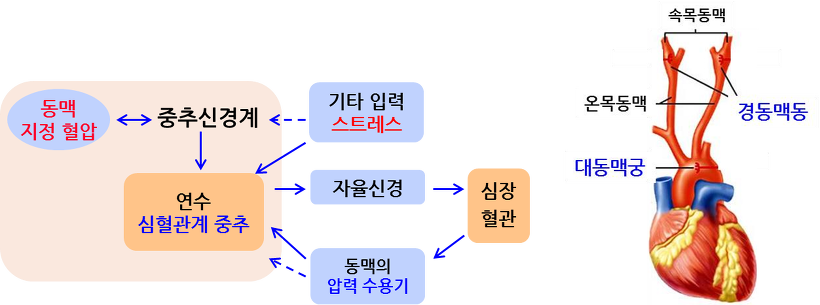
Figure 18. Global blood flow regulation mechanism
The dashed line represents the feedback circuit associated with the specified blood pressure adjustment
① Medulla oblongata: the autonomic nervous system control center
○ PH detection of cerebrospinal fluid → control of breathing and circulation
○ Since H+ does not pass through BBB, pH change is detected through simple diffusion of CO2 and carbonate acid-base reaction.
② Arterial Baroreceptors
○ Located in the aortic arch and carotid sinuses, they send signals to the medulla oblongata.
○ The carotid sinus is a more effective baroreceptor than the aortic arch.
③ Blood Flow Control Process
○ 1st. Increased blood pressure → Arterial baroreceptors act on the medulla oblongata.
○ 2nd. The medulla oblongata directly stimulates the parasympathetic nervous system.
○ Parasympathetic nerve terminals: release acetylcholine, resulting in delayed heart rate.
○ 3rd. The medulla oblongata acts on inhibitory interneurons in the spinal cord to suppress the sympathetic nervous system.
○ Sympathetic nerve terminals: release epinephrine, which increases heart rate.
○ Cardiotonic agent: epinephrine
○ 4th. ↑ Parasympathetic activity, ↓ Sympathetic activity: arteriolar dilation, delayed pacemaker activity, decreased cardiac output.
④ Example 1. Astronauts
○ Although the actual water volume is low, the body is misled into thinking there is excess fluid → increased urine output.
○ Recovery mechanism: ↑ Sympathetic activity → prevents peripheral blood pooling → conserves body fluids.
⑤ Example 2. Orthostatic Hypotension
○ Due to gravity, venous return ↓ → cerebral blood flow ↓ → symptoms of dizziness/faintness.
○ Recovery mechanism: ↑ Sympathetic activity → prevents peripheral blood pooling → conserves body fluids.
⑶ Local regulation: Contraction and Relaxation of Arterial Smooth Muscle
① Arterial smooth muscle is controlled by the autonomic nervous system
② General: When the sympathetic nervous system is activated, arterioles leading to visceral organs constrict, while arterioles leading to skeletal muscles dilate.
③ Transient hyperemia: Arterioles near tissues with low oxygen partial pressure and high carbon dioxide partial pressure dilate, increasing blood flow.
④ Active hyperemia: Blood flow supply is proportional to metabolic changes caused by local activity (e.g., exercise).
⑤ Reactive hyperemia: Increased blood flow in response to a prior reduction in blood flow.
○ Endothelin: A vasoconstrictor
Figure 19. Aortic smooth muscle regulation mechanism
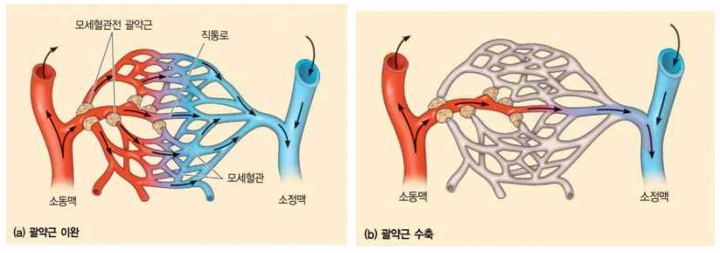
⑷ Local regulation: Capillary Microcirculation Control
① Contraction and Relaxation of Total Capillary Sphincter or Endothelial Cells
○ Relaxation of the arterioles increases full load → increases capillary blood pressure
Figure 20. Mechanisms of Microcirculation Control of Capillaries
② Quantitative explanation: Blood flow resistance (R) is inversely proportional to the fourth power of the vessel radius (r).
③ Even a slight adjustment of the radius of a specific capillary can easily regulate the blood flow through that vessel as well as other associated capillaries.
⑸ Local regulation: Histamine
① Capillary dilation during inflammatory response
② Increased vascular permeability
③ Increased blood flow to the injured area (↑ complement protein influx)
④ Relaxation of smooth muscle
6. Blood Coagulation
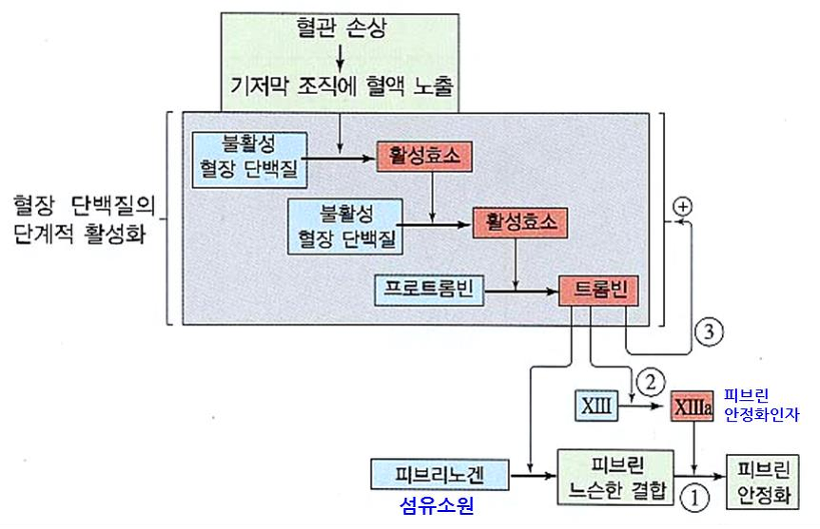
⑴ Exogenous coagulation: Coagulation outside the vessel. General coagulation process
① 1st. Endothelial Surface Changes: Exposure of collagen on the endothelial cell surface
② 2nd. Primary hemostasis
○ 2nd-1st. Platelets adsorb to collagen in connective tissue and physically block
○ 2nd-2nd. Secretion of substances by bound platelets that promote the adhesion of nearby platelets
③ 3rd. Secondary hemostasis: Clumps blood cells in the blood while forming fibrin aggregates. Platelet plug formation
Figure 21. Blood clotting process
○ 3rd-1st. Fibrin Formation by Multistage Enzyme Reaction of Platelets, Damaged Cells, and Plasma Coagulation Factors
○ 3rd-1st-1st. Secretion of clotting factors such as thrombokinase from damaged tissue cells
○ 3rd-1st-2nd. Blood coagulation factor is activated by Ca2+.
○ 3rd-1st-3rd. Activated coagulation factor activates prothrombin to thrombin together with Ca2+.
○ 3rd-1st-4th. Thrombin activates fibrinogen (in the sol state) into fibrin (in the gel state).
○ In blood coagulation, thrombin and other plasma proteins are proteolytic enzymes.
○ 3rd-2nd. As fibrin clumps together, a fibrin clot (thrombus) forms, creating a platelet plug that seals the wound site.
④ 4th. Vasoconstriction: Aggregated platelets contract smooth muscle, synthesizing thromboxane A2 and releasing chemical mediators
○ 4th-1st. Arachidonic acid → prostaglandins: cyclooxygenase is involved
○ 4th-2nd. Prostaglandins → Thromboxane: thromboxane synthetase is involved
⑤ 5th. Wound closure
○ 5th-1st. PDGF secretion from platelets
○ 5th-2nd. PDGF receptors on epithelial cells show tyrosine kinase activity
○ 5th-3rd. Increased collagen fibers in fibroblasts → wound closure
⑵ Endogenous coagulation: Coagulation within blood vessels
① Involves Hageman factor.
② Generally speaking, blood coagulation refers to exogenous coagulation, not endogenous coagulation.
⑶ Regulation of blood clotting
① Vitamin K: Essential for blood clotting; other vitamins are independent of blood clotting
② Prostacyclin (PGI2), Nitric Oxide (NO): Inhibit platelet aggregation
○ Generated from endothelial cells
○ Prevention of platelet plug formation in areas other than the site of injury
③ Aspirin
○ Exerts an anticoagulant effect by inhibiting cyclooxygenase, which is involved in thromboxane synthesis
○ Positive effects: antipyretic and analgesic action, prevention of heart attacks, thrombolytic effect
○ Side effects: gastric ulcers (related to mucous membrane formation), cases of death due to inability to stop bleeding during surgery, gastrointestinal bleeding, cerebral hemorrhage
④ Heparin, hirudin: Anticoagulant action by inhibiting the activation of protein lyase
○ Heparin: synthesized by mast cells, with most of its carboxyl groups carrying a negative charge; present in the liver.
○ 1st . Heparin and anti-thrombin III bind
○ 2nd. The three-dimensional structure of antithrombin changes
○ 3rd. Heparin and antithrombin conjugates irreversibly bind to thrombin
○ 4th. When antithrombin binds to thrombin, its binding affinity for heparin decreases, causing it to dissociate.
○ 5th. Heparin is recycled and combined with another antithrombin
○ Types: Unfractionated heparin, Enoxaparin, Daltaparin, Tinzaparin
○ Hirudin: an anticoagulant substance found in leeches, secreted to prevent the ingested blood from clotting.
⑤ Warfarin: Competitive inhibitor of vitamin K, anticoagulant action by inhibiting prothrombin formation
⑥ EDTA, sodium citrate, sodium oxalate: Anticoagulant by removing calcium
⑦ Plasmin: Blood clot removal
⑧ Xa inhibitor
○ Fondaparinux
○ Rivaroxiban
○ Apixaban
⑨ Direct inhibitor to thrombin
○ Dalbigatran
○ Bivalirudin
○ Argatroban
⑷ Blood type and blood coagulation
① ABO Blood Type
○ Type A standard serum (anti-B): contains antigen A and agglutinin β.
○ Type A blood recognizes substances similar to antigen B—produced by Escherichia coli—as foreign, and produces agglutinin β.
○ Type B standard serum (anti-A): contains antigen B and agglutinin α.
○ Type B blood recognizes substances similar to antigen A—produced by Escherichia coli—as foreign, and produces agglutinin α.
○ Reaction with standard sera:
○ Agglutination occurs between antigen A and agglutinin α, and between antigen B and agglutinin β.
○ Type A blood: has antigen A and a trace amount of agglutinin β, and agglutinates with type B standard serum (anti-A).
○ Type B blood: has antigen B and a trace amount of agglutinin α, and agglutinates with type A standard serum (anti-B).
○ Type AB blood: has both antigen A and antigen B but no agglutinins; agglutinates with both type A and type B standard sera.
○ Type O blood: has no antigens but has both agglutinin α and agglutinin β; does not agglutinate.
○ Transfusion:
○ Type A can donate only to types A and AB.
○ Type B can donate only to types B and AB.
○ Type AB can donate only to type AB.
○ Type O can donate to types AB, A, B, and O.
○ Example 1: Transfusing type O blood into type A
○ Antibodies in type O blood are in trace amounts, so they do not cause a major problem.
○ From the type A recipient’s perspective, there are no foreign antigens, so it is not problematic.
○ Example 2: Transfusing type A blood into type O
○ Antibodies in type A blood are in trace amounts, so they do not cause a major problem.
○ From the type O recipient’s perspective, the foreign antigen A is introduced, leading to the production of large amounts of α antibodies, causing an agglutination reaction → death.
○ Plastic blood: not dependent on blood type.
○ Structure of blood type antigens: determined by the sugar attached after adding fucose to the red blood cell surface.
② MNS Blood Type
③ Lutheran Blood Groups
7. Cardiovascular disease
⑴ Arteriosclerosis: Oil in blood vessels causes arteries to harden
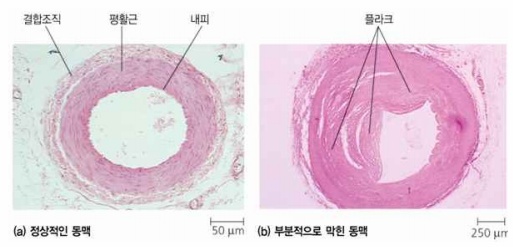
Figure 22. Arteriosclerosis
① Definition: a condition in which fat builds up inside blood vessels, causing arteries to harden.
○ CAD (coronary artery disease): a disease of the coronary arteries.
○ Heart attack: caused by blockage of the coronary arteries, which stops the supply of oxygen to the heart muscle and leads to the death of heart muscle cells.
② 1st. Lipoproteins, such as LDL, become entangled in the arterial endothelium
○ case 1: Cholesterol deposits on damaged sites after damage to the vessel’s inner wall
○ case 2: Cholesterol deposition around the inside of blood vessels: Decreased elasticity of blood vessels
③ 2nd. Macrophages ingest it and transform into lipid-rich foam cells.
④ 3rd. Plaque (atheromatous deposit) formation: when extracellular matrix components (such as collagen) are secreted, the lipoprotein mass enlarges.
⑤ 4th. T lymphocytes and smooth muscle cells of the vessel wall also join the plaque.
⑥ 5th. Part of the smooth muscle cells form a fibrous cap that separates the plaque from the blood
⑦ 6th. Foam cells in plaque die and release cellular residue and cholesterol
○ If a plaque ruptures, a thrombus forms in the artery.
○ If a plaque does not rupture but continues to grow, it can block the artery.
○ When the coronary artery is blocked, it causes angina pectoris.
⑧ 7th. It takes about 40 years for hematoma and thrombus formation to occur. ChatGPT에게 묻기
⑨ Type 1. Atherosclerosis: CD40-CD40L is involved.
⑩ Type 2. Gaucher’s disease
⑪ Type 3. Niemenn-Pick disease
⑵ Primary hyperlipidemia: One of genetic diseases
① Type Ⅰ: Lipoprotein lipase deficiency
② Type Ⅱa: Defective LDL receptor
③ Type Ⅱb: Unknown cause
④ Type Ⅲ: Abnormal apoplipoprotein E
⑤ Type Ⅳ: Unknown cause
⑥ Type Ⅴ :Deficiency of apoplipoprotein C
⑶ Stroke
① Definition: A condition in which blood cannot flow through the cerebral blood vessels, causing tissue death due to lack of oxygen.
○ Ischemic stroke: Occurs when an artery in the head becomes blocked → blood supply to downstream tissue is cut off.
○ Hemorrhagic stroke: Occurs when an artery in the head ruptures.
○ If treated within three hours, the effects of a stroke can be completely reversed.
② Can also be caused by a blood clot (thrombus).
⑷ Hypertension
① Defition: Symptoms with a contraction pressure of at least 140 mmHg and a relaxation pressure of at least 90 mmHg
② Cause: Increased cardiac output, increased peripheral resistance
③ Characteristic: In patients with hypertension, the pressure receptors (baroreceptors) in the carotid artery and aorta perceive the high blood pressure as normal, resulting in a failure to initiate the baroreceptor reflex to lower blood pressure.
⑸ Anemia
① Overview
○ Definition: A condition in which red blood cells are unable to effectively carry oxygen.
○ More specifically, it refers to cases where the hemoglobin level or hematocrit level in the blood — in other words, the concentration of red blood cells — is lower than normal.
② Anemia due to impaired hematopoiesis: Includes hemolytic anemia (e.g., sickle cell anemia) and other conditions with a reduced number of red blood cells. Red blood cell production can also decrease after blood transfusions.
③ Iron-deficiency anemia
④ Pernicious anemia (e.g., caused by a deficiency of vitamin B12)
⑤ Aplastic anemia: Anemia resulting from damage to bone marrow production function. It cannot be treated with medication and requires blood transfusions.
⑥ Renal anemia: Anemia caused by kidney failure; it cannot be treated with medication and requires blood transfusions.
⑹ Cardiomyopathy
① Type 1. DCM (Dilated Cardiomyopathy): Left ventricular dilation with normal left ventricular wall thickness.
② Type 2. HCM (Hypertrophic Cardiomyopathy): Increased left ventricular wall thickness; associated with mutations in sarcomere genes.
⑺ Lymphatic System–Related Diseases
① CLL (Chronic Lymphocytic Leukemia): Characterized by small lymphocytes.
② FL (Follicular Lymphoma):
○ Grade I: Between 0 and 5 centroblasts
○ Grade II: Between 6 and 15 centroblasts
○ Grade III: More than 15 centroblasts
○ Grade III-A: Centrocytes are present
○ Grade III-B: Centroblasts form clusters
③ MCL (Mantle Cell Lymphoma)
⑻ Brugada Syndrome: A rare disorder in which the heart suddenly stops beating (sudden cardiac arrest).
8. Cardiovascular Diagnosis
⑴ Diagnosis of CAD (Coronary Artery Disease)
① Invasive methods
○ Invasive coronary angiography: Traditional gold standard; offers high resolution.
○ FFR (Fractional Flow Reserve): Distal coronary pressure ÷ proximal coronary pressure.
○ IVUS (Intravascular Ultrasound): The catheter tip emits ultrasound waves.
○ OCT (Optical Coherence Tomography): Detects lesions at a higher resolution than IVUS; more advanced than NIRS.
② Direct visualization methods among non-invasive techniques
○ CAC (Coronary Calcium Score)
○ EBCT (Electron Beam CT)
○ MDCT (Multidetector CT)
○ Magnetic Resonance Angiography
③ Functional imaging techniques among non-invasive methods
○ Myocardial perfusion scintigraphy: Uses SPECT and PET.
○ SE (Stress Echocardiography)
○ CMR (Cardiac MRI)
○ CT Angiography: Performed after intravenous injection, followed by image reconstruction.
⑵ Cholesterol level assessment: Measure LDL/HDL levels.
⑶ Inflammatory response assessment: Inflammation plays a critical role in atherosclerosis and thrombus formation.
① Treatment: Aspirin → prevents recurrence of heart attack and stroke.
② CRP (C-reactive protein) measurement: Synthesized in the liver; blood levels increase during inflammatory responses.
⑷ Blood pressure assessment: In hypertension, arterial wall damage promotes plaque formation.
⑸ Myocardial perfusion agents
| ²⁰¹Tl | ⁹⁹ᵐTc-MIBI | ¹⁵O-H₂O | ¹³N-NH₃ | ⁸²Rb | |
|---|---|---|---|---|---|
| 1st-pass EF | 0.85 | 0.65 | 1.0 | 0.9 | 0.6 |
| linearity | good | fair | excellent | good | good |
| energy | 70 keV | 140 keV | 511 keV | 511 keV | 511 keV |
| uptake mechanism | Na/K ATPase | mitochondria membrane | free diffusion | diffusion metabolism | Na/K ATPase |
| half time | 74 hr | 6 hr | 2 min | 20 min | 1.2 min |
Table 2. Myocardial perfusion agents
⑹ Coronary Flow Reserve (CFR)
① A compensatory mechanism in which blood vessels dilate in response to changes in pressure to maintain a constant blood flow.
② Because there is a limit to how much the vessels can dilate, there is a certain pressure at which blood flow can no longer remain constant and instead decreases.
③ In people with angina, coronary flow reserve is reduced.
Input: 2015.7.18 00:07
Modify: 2019.2.10 22:34